How Do Federal Shutdowns Impact EMS? National Survey Results

Executive Summary
A recent federal government shutdown and a series of federal policy changes has produced immediate and near-term harm to EMS agencies across the United States.
- Medicare claims processing and temporary ambulance add-ons have been disrupted or put at risk.
- FEMA and other grant programs that fund equipment, staffing, and training have been cancelled or delayed
- Health-system changes tied to federal waivers (e.g., hospital-at-home and telemedicine flexibility) have been destabilized.
All of these changes amplify financial strain and operational risk for already fragile EMS systems, especially rural and volunteer services. Additionally, delays in processing Medicare claims for ambulance services has caused significant financial burdens on EMS agencies already struggling with a fragile economic climate.
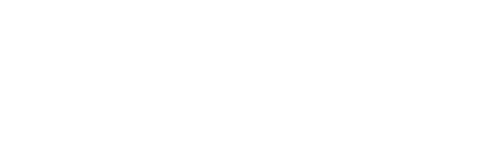
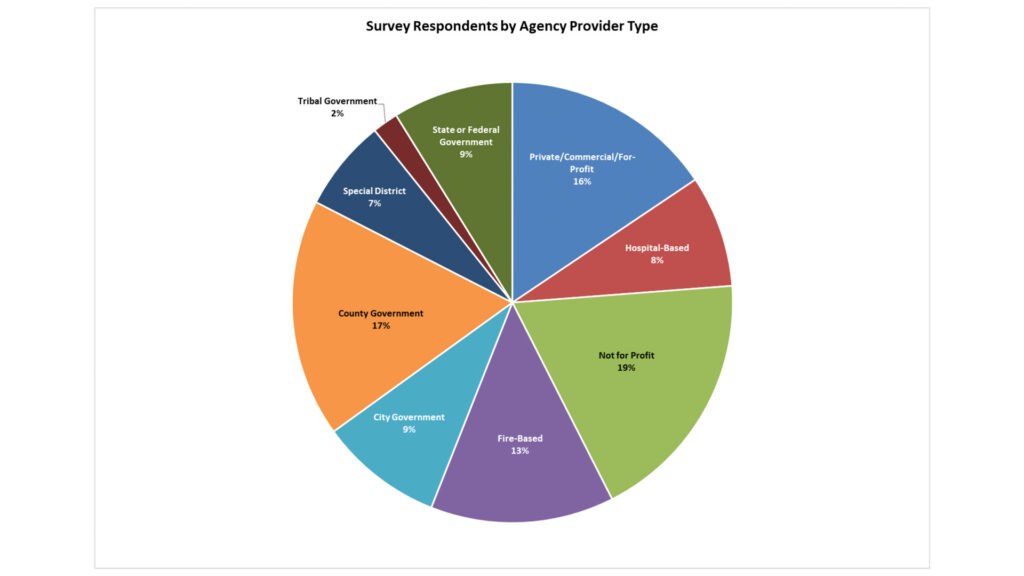
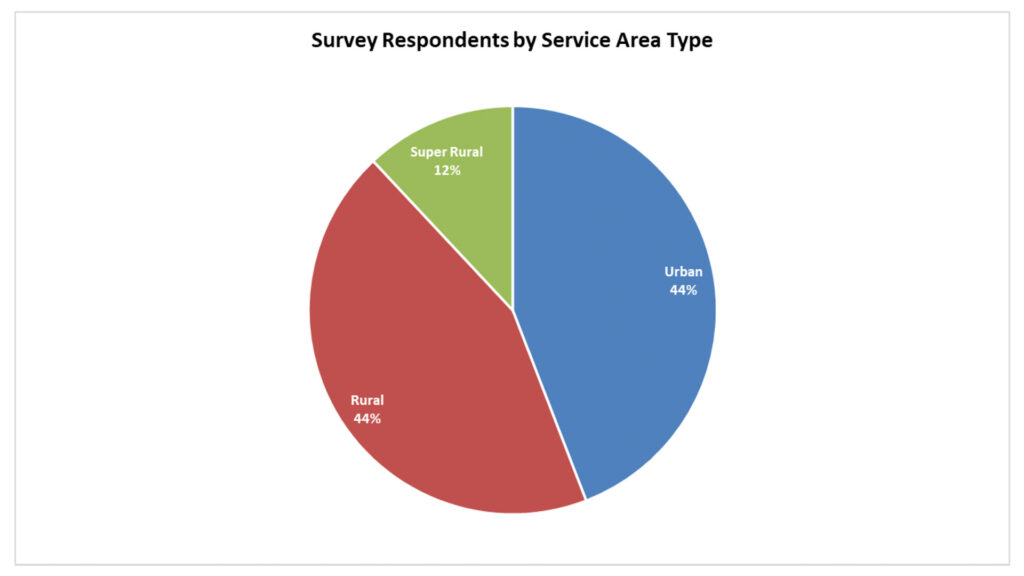
A recent survey by the National Association of Emergency Medical Technicians, supported by numerous national fire and EMS organizations, chronicles the real impact of the government shutdown on day-to-day essential EMS operations. The survey generated over 400 responses from agencies across the U.S.
Background: Why EMS is Vulnerable
EMS is a high-fixed-cost delivery model that communities reply on to be present at all times. Many ground ambulance services rely heavily on Medicare reimbursements and on periodic federal grants (AFG/SAFER, FEMA grants) to buy vehicles, lifesaving technology, radios, training, and to fund overtime or hires. Delays or reductions in federal funding therefore translate quickly into cash-flow problems, canceled purchases, difficulty meeting payroll, and potential service reductions. It is important to note that the elderly make up a disproportionate share of ambulance patients due to the increase in disease as people age, thus making the EMS system both highly dependent on Medicare and very vulnerable to Medicare changes.
The federal shutdown has resulted in furloughed staff who administer grant programs essential to EMS functions and has triggered uncertainty of Medicare payments and extensions/waivers. In addition, administrative reprioritizations in agency spending and reductions in the federal workforce have left many grant programs delayed or terminated. The combination of these changes have significant effects to local providers that cannot absorb losing essential federal government functions.
Impacts on EMS
Payment and cash-flow disruptions
CMS guidance during recent shutdown activity has led to holds or delayed release of Medicare claims in some categories. Revenue was immediately reduced on many transports when the congressional authorization for temporary Medicare “add-ons” for ground ambulance services (urban/rural/super-rural bonuses) lapsed. Rural and Medicare-heavy agencies were the most exposed. The expiration of the add-ons exacerbated longstanding financial vulnerability since Medicare already pays EMS agencies less than it costs to deliver service.
Health-system downstream effects that increase EMS demand
Waiver-dependent programs (e.g., Medicare hospital-at-home, telehealth flexibilities) paused or scaled back during the shutdown have forced patients back into emergency departments and inpatient beds in some systems — increasing 911 call volume and ambulance transports and lengthening hospital turnaround times. In addition, some mobile integrated health programs (MIH) that involved EMS agency clinicians in less expensive at home care models became immediately unfunded.
Grants, training, and capital projects delayed
FEMA and HRSA-administered grant programs (Assistance to Firefighters Grant, SAFER, etc.) and other federal grant review/award processes have been delayed or frozen during prior shutdowns when agency staff were furloughed, causing postponed equipment purchases, hiring rounds, and training schedules. Throughout 2025 federal administrative agency restructurings have resulted in cancellations and significant delays of many grants. This slows modernization, reduces capacity, and stifles innovative programs at the same time demand is rising.
Population-specific health
Rural, tribal, and low-income communities are disproportionately affected: they rely more on Medicare revenue, are more likely to have volunteer or thinly funded services and have fewer local budgetary buffers to cover federal funding interruptions. The result: service loss risk concentrates where alternatives are sparse.
Conclusion
The federal government shutdown and other federal administrative changes has created a national operational crisis for EMS. Payment holds, grant delays and cancellations, disrupted federal coordination, and instability in related health programs combine to threaten ambulance system solvency and response capacity — especially in rural and resource-constrained communities. Rapid legislative and administrative fixes that prioritize continuity of ambulance payments, grant administration, and disaster response are essential to prevent service reductions that would directly endanger public safety.
Survey Results
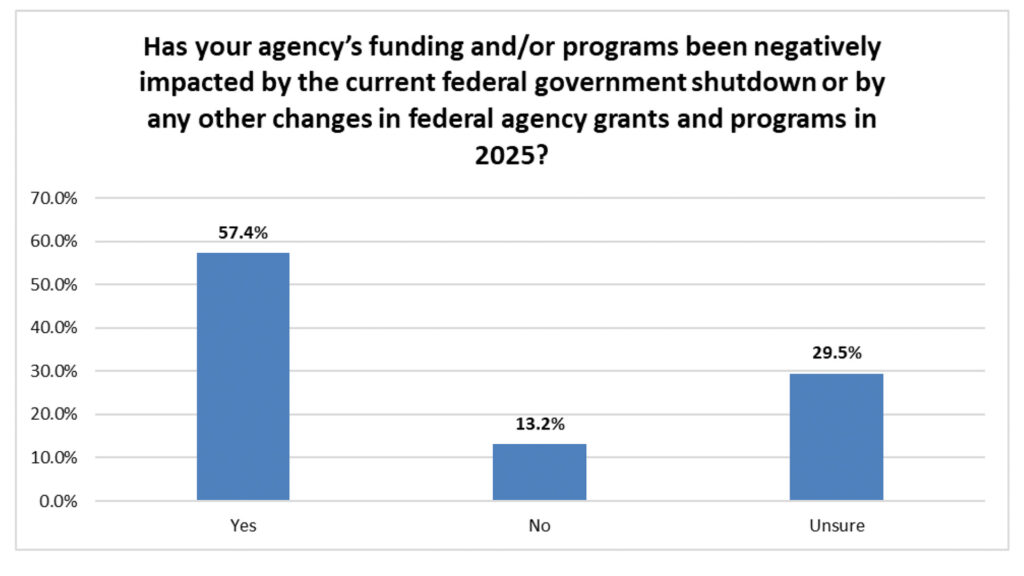
The 408 agencies responding to the survey identified 4 main themes related to the adverse impact of the government shutdown on EMS systems:
- Financial strains due to Medicare claim submissions and payment delays, including missed or delayed payrolls
- Loss of federal grant funds or contracts delayed during 2025 and have had to delay or postpone projects or programs
- Delays in EMS clinician training due to the unavailability of federal education resources
- EMS-based Mobile Integrated Health/Community Paramedicine (MIH/CP) programs have had consequences due to changes to other health programs such as telehealth coverage and hospital at home
“We are a rural agency that relies on Medicare payments. Around 60% of our income is from that payment source. As a 911 service, we have to respond and we have a budget for payroll and equipment. We are cutting back on crews to not get so far behind that we can’t catch up. We are still paying the staff and buying supplies, but no reimbursements for over a month. This is not helping our community at all, and we are talking about how we can keep this up.”
“We are currently unable to onboard members because the required Federal Incident Command classes being unavailable.”
“The delay in processing Medicare claims between the pause at CMS and concern over having to re-work all the claims due to the extenders have greatly affected cash flow.”
“Our pay has been delayed almost every week for over a month. Crews have quit and the company couldn’t pay our health insurance premiums.”
“We were supposed to get new ambulances, but can’t due to budgetary restrictions. Our trucks are constantly breaking down.”
“Cash on hand for daily operations is running dangerously close to drying up.”
“Due to the government shutdown, we have been worried about making payroll and performing vehicle maintenance. The end of the year timing is very hard with such tight budgets, especially being part of county systems that has levy limits due to State laws.”
Sources
- https://www.congress.gov/crs-product/RL33375
- https://www.ems1.com/billing-and-administration/government-shutdown-what-it-means-for-ambulance-services
- https://www.politico.com/news/2025/10/14/hospital-at-home-program-collateral-damage-of-the-shutdown-00602997
- https://www.myjournalcourier.com/news/article/west-central-illinois-ambulances-see-21136288.php
- https://www.hrsonline.org/resource/2025-government-shut-down-medicare-claims-impact
- https://nlihc.org/resource/impact-government-shutdown-disaster-response