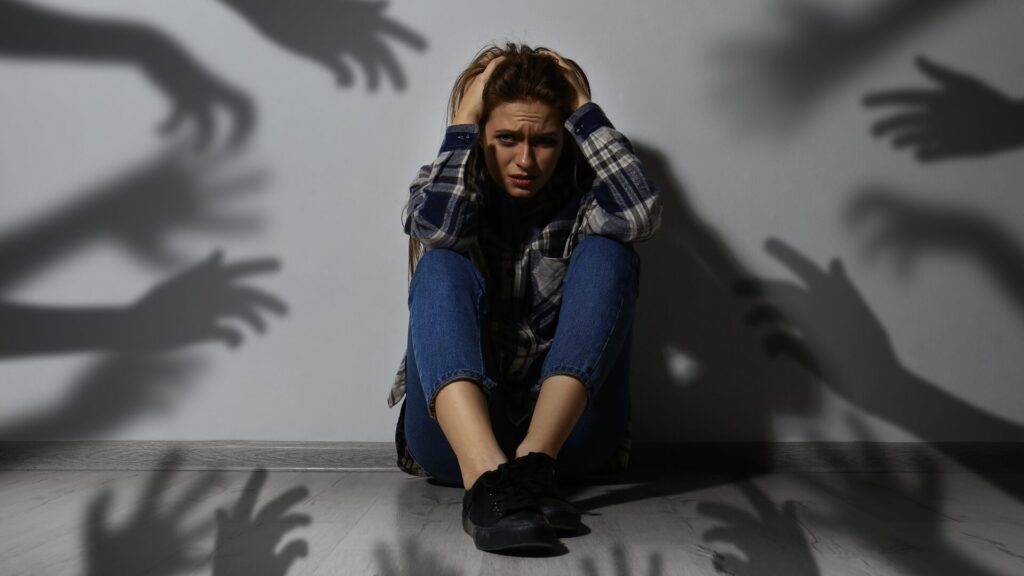
Saving More Lives with Prehospital Blood Products
Some EMS agencies are at the forefront of this trauma system initiative
You arrive on the scene of a motor vehicle collision to a bleeding and unresponsive patient. This is a leading cause of trauma-related death and a scene all too familiar to those working in EMS. Knowing the patient is likely hemorrhaging and time is of the essence, you do your best to control the bleeding and replace the lost blood with fluids, likely crystalloids, to correct the hypovolemia and achieve hemodynamic stability. Upon arrival at the hospital, the patient receives continued resuscitation with blood transfusions, the gold standard treatment for hemorrhagic shock: replacing lost blood volume with whole blood, which contains red blood cells, platelets, clotting factors, and proteins. If your patient survives, they may be faced with a lengthy stay in the intensive care unit battling cardiac and pulmonary complications related to crystalloid use in hemorrhagic shock.
Research suggests that the overuse of crystalloids in hemorrhagic shock increases the risk of many complications, including death. What if you could increase survivability and decrease complications by starting a blood transfusion on-scene or during transport to the hospital? This option is the budding reality for some EMS agencies at the forefront of trauma care and hemorrhagic shock management.
LIFE-LIMITING HEMORRHAGIC SHOCK
Hemorrhage is the leading cause of preventable death in trauma patients, with nearly half of these patients dying in the prehospital setting. Hemorrhagic shock is caused by significant blood loss, which depletes intravascular volume, ultimately leading to multisystem organ failure and, if left untreated, death. Hemorrhage most often occurs after blunt or penetrating trauma, though it is also common after gastrointestinal, obstetric, or surgical bleeding.
Blood is the answer
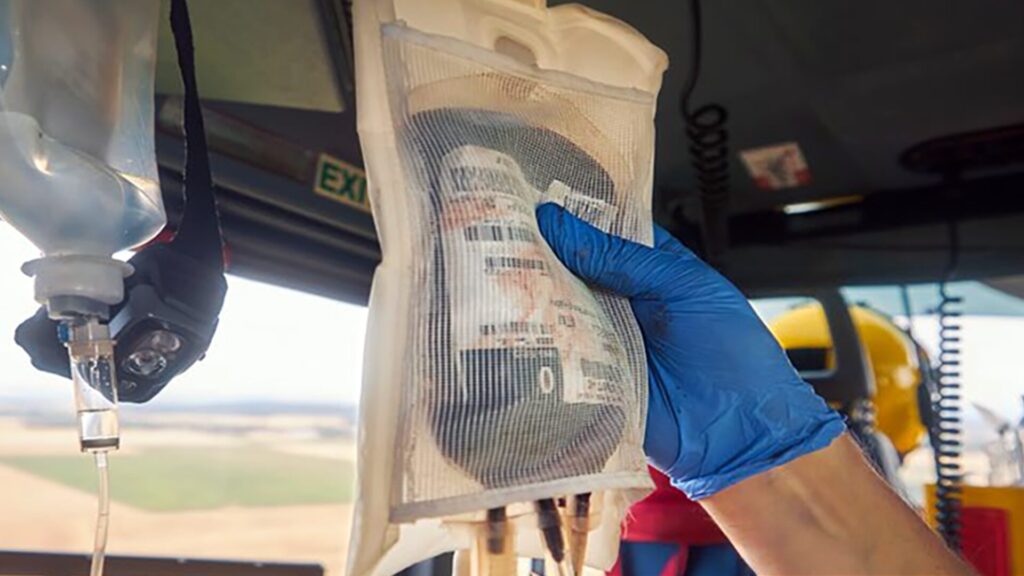
Common blood products used in resuscitation include crystalloid fluids, blood components, and whole blood. Crystalloid fluids, such as normal saline and Lactated Ringers, are water-based solutions containing salt and other minerals. By contrast, blood components are isolated parts of human blood, including red blood cells, white blood cells, platelets, and plasma. Whole blood contains a balanced ratio of each blood component, making it ideal for hemorrhagic shock resuscitation.

THE MILITARY LEADS THE WAY
The military has long understood the importance of replacing lost blood volume with blood products. As early as the Civil War, the military administered blood to injured service members on the battlefield. Technology and logistics made this a difficult reality, but in 1865, two whole blood transfusions were attempted on soldiers wounded under fire. The concept of blood typing emerged, and by World War I, both cold-stored and warm whole-blood transfusions were administered to wounded soldiers. Throughout the early 1900s, the use of blood products for combat casualty care continued to increase. In the 1940s, the U.S. Surgeon General advised the Armed Forces to use blood products to treat shock whenever possible. Blood products saved many lives and decreased the rates of combat casualties from 8.1% to 3.3% between World War I and World War II.
Advancements in technology
Advancements in medical research and technology throughout the 1950s, including the ability to separate blood into its components, improved the efficacy and safety of blood transfusions. Through the end of the Vietnam War in the 1970s, low-titer group “O” whole blood was used for mass transfusions in the setting of hemorrhagic shock. This type of whole blood can be safely transfused into people of any blood type, reducing the risk of a transfusion reaction. Following the Vietnam War, however, the guidelines for hemorrhagic shock management shifted to crystalloid fluids, ultimately leading to the divergence from whole blood.
The turn of the century
Mounting evidence in the late 1990s and early 2000s suggested worsening patient outcomes with the current fluid resuscitation strategy. The importance of replacing lost blood with blood products in cases of hemorrhagic shock re-emerged. Whole blood returned to the conversation as new research suggested improved outcomes with whole blood as opposed to blood components during the Iraq and Afghanistan wars. Today, whole blood is a staple resuscitation fluid in military trauma response. During a recent American College of Surgeons news conference, Dr. Jennifer Gurney, MD, FACS, COL U.S. Army and Department of Defense Joint Trauma System Chief, noted that helicopters do not travel downrange on missions without whole blood. Blood products are recognized as essential, lifesaving prehospital trauma treatments

HISTORY IN THE MAKING
Bridging military prehospital trauma response to the civilian sector is not new. In 2013, public safety organizations responded to the increase in mass casualty shootings by developing a set of guidelines known as the Hartford Consensus, with the goal of increasing survivability. The Hartford Consensus borrowed concepts from the military in their framework, “THREAT.” The acronym refers to threat suppression, hemorrhage control, rapid extraction to safety, assessment by medical providers, and transport to definitive care. The Hartford Consensus is part of a larger plan to integrate military and civilian trauma responses and build a national trauma care system. The overarching goal is to achieve zero preventable deaths. The Hartford Consensus guidelines emphasize prompt EMS intervention and bleeding control, but a crucial next step in reducing preventable deaths is providing prehospital blood products to patients experiencing hemorrhage.
Since its inception in 2021, New Orleans EMS’ prehospital blood program has administered 290 units of packed red blood cells, or about one transfusion every three to four days.Saving more lives with prehospital blood
After Neil Niemczyk’s six-year-old daughter suffered a post-tonsillectomy hemorrhage in Palm Beach County, Florida, a prehospital blood transfusion saved her life. In an interview with NBC News, he notes, “30 seconds after that first pump, Izzy went from being unconscious to being alert and looking around.” Palm Beach County is one of over 180 EMS agencies changing the landscape of trauma system care by administering prehospital blood products. There are numerous stories with similar accounts. Since its inception in 2021, New Orleans EMS’ prehospital blood program has administered 290 units of packed red blood cells, or about one transfusion every three to four days. Major Thomas Dransfield credits the program with the ability to “deliver a more hemodynamically stable patient to the trauma team.” Imagine being able to improve the level of consciousness and stabilize the vital signs of your trauma patient shortly after you arrive on scene. Colorado Springs EMS recently established its prehospital blood program, saving 32 lives in the first 100 days of the program, including one woman who hemorrhaged during labor. Practitioners initiated blood within just eighteen minutes of her husband’s 911 call, saving the lives of both mother and baby.
Hemorrhaging patients who receive blood before arriving at the hospital have a fourfold increase in 24-hour survival.Fourteen Minutes
The data is clear: hemorrhaging patients who receive blood before arriving at the hospital have a fourfold increase in 24-hour survival. For every one-minute delay in blood product resuscitation in hemorrhagic shock, the odds of 30- day mortality increase by 2%. Receiving blood within fourteen minutes of injury is associated with improved outcomes. Fourteen minutes can mean the difference between life and death. Notably, the national average EMS response time is seven minutes, with varying on-scene and transport times. Therefore, to achieve optimal outcomes, patients should receive blood shortly after EMS arrives on scene and certainly before they arrive at the hospital. Today, under 2% of EMS agencies carry blood, and just 1% of patients who could receive prehospital blood actually get it. Why?

OVERCOMING HURDLES
EMS agencies with active blood programs have overcome many barriers to starting their programs. Major Thomas Dransfield of New Orleans EMS remarks that despite initial pushback from naysayers of the prehospital blood program, “the results were undeniable proof that it is beneficial without extending scene/transport times.” Saving the lives of hemorrhaging patients makes the prehospital blood program a worthwhile investment. The Prehospital Blood Transfusion Initiative Coalition is an industry-wide, multidisciplinary initiative to help overcome barriers to prehospital blood administration. According to Dr. Jon Krohmer, MD, FACEP, FAEMS, the steering committee chair for the coalition, three significant barriers prevent civilians nationwide from receiving prehospital blood: reimbursement, scope of practice, and blood supply.
Reimbursement
For years, EMS has been chronically underfunded, and prehospital blood is not yet a reimbursable expense. The overhead cost for supplies to support blood administration averages $15,000- $20,000, with each transfusion costing an average of $1,000-$1,500. Yet, most agencies are reimbursed less than $1000 per transport. So, where does the funding come from? Many of the agencies with blood programs pull this funding from their operational budget or receive grant funding. Recently, the Centers for Medicare and Medicaid Services (CMS) proposed adding whole-blood transfusions to approved advanced life support (ALS) level-two procedures. Although CMS did not designate reimbursement for the procedure, the proposal itself is significant.
Scope of Practice
Historically, blood transfusions were outside the scope of practice for EMS paramedics. Today, 40 states allow EMS practitioners to initiate blood transfusions in the field, and that number continues to rise as data signifies the importance of timely transfusions. Dr. Krohmer notes, “It is a safe intervention for EMS practitioners to initiate and conduct. There are certainly possibilities of adverse reactions, but those are extremely rare, and EMS practitioners can identify and treat those reactions.” The Prehospital Blood Transfusion Initiative Coalition is actively working with the remaining states to overcome individual barriers.
Blood Supply
Most agencies with blood protocols work with hospital blood banks or community blood centers to obtain the needed blood, though blood availability is a challenge nationwide. While some skeptics suggest that prehospital blood programs may drain the national blood supply, the literature suggests that trauma patients who receive prehospital blood have a decreased need for subsequent blood transfusions. Some organizations, like New Orleans EMS, partner with local blood suppliers and work with the community to increase donor contributions. Consequently, prehospital blood programs may even boost blood supply.

LOOKING FORWARD
What does the future landscape of prehospital blood programs look like? While it may not be feasible for whole blood to be stored in every ambulance nationwide, freeze-dried plasma is a promising alternative: it is easy to carry, has no specific storage needs, and has a long shelf life. It is currently available in Europe, and the Food and Drug Administration (FDA) recently approved its emergency use in the military. Dr. Krohmer believes that freeze-dried plasma could be stored on most ambulances and provide bridge therapy until whole blood or red blood cells arrive. Expanding prehospital blood product availability is pivotal as we move towards the goal of zero preventable deaths with a national trauma care system. Dr. Krohmer believes we will continue to see an increase in the number of EMS agencies with blood programs. He considers this “the most significant clinical intervention we’ve seen for EMS practitioners in decades.” Only time will tell what the future holds as the trauma system continues to evolve.